THE CURRENT PARADIGM AND AGE-ASSOCIATED DISORDERS
“The science of today is the technology of tomorrow.”
Edward Teller
The first of Thomas Kuhn’s three prerequisites for paradigm shift is dissatisfaction with the prevailing paradigm. A number of essays in this website discuss how the current aging paradigm is simply not an accurate depiction of reality. Other essays discuss why the current paradigm not only isn’t an accurate depiction of reality but, why, since it is inconsistent with the principles of natural selection, it’s impossible for it to be consistent with reality. Since a paradigm is the set of preconceptions that is assumed to represent reality, the fact that the current paradigm is inconsistent with reality is sufficient cause to be dissatisfied with it.
Infectious Disease Approach
Although using the infectious disease approach for age-associated degenerative diseases is misguided from a scientific standpoint, the approach has proven to be remarkably lucrative for the pharmaceutical industry. The pharmaceutical industry’s approach to developing pharmaceutical interventions intended to target age-associated degenerative diseases is discussed in the essay entitled “Pharmaceutical Interventions for Age-Associated Diseases.”
Risk Factors
In the absence of an identifiable actual cause for age-associated degenerative diseases, the concept of “risk factor” has been substituted. The indiscriminate use of that term, and the practice of equating risk factor to cause, has had unfortunate consequences. When dealing with infectious diseases, inherent in the concept of “cause” is the understanding that if the cause of the disease (the pertinent pathogen) is eliminated, the disease will either be prevented or cured. Most of the recognized environmental risk factors for age-associated degenerative diseases are factors that accelerate the rate at which intrinsic damage is inflicted upon the subject. Examples include smoking, excessive alcohol consumption, stress, obesity, etc. But we know that none of these factors are the root cause of age-associated degenerative diseases, because even if a subject neutralized or eliminated all such factors, there can be no assurance that the subject will be immune from those disorders.
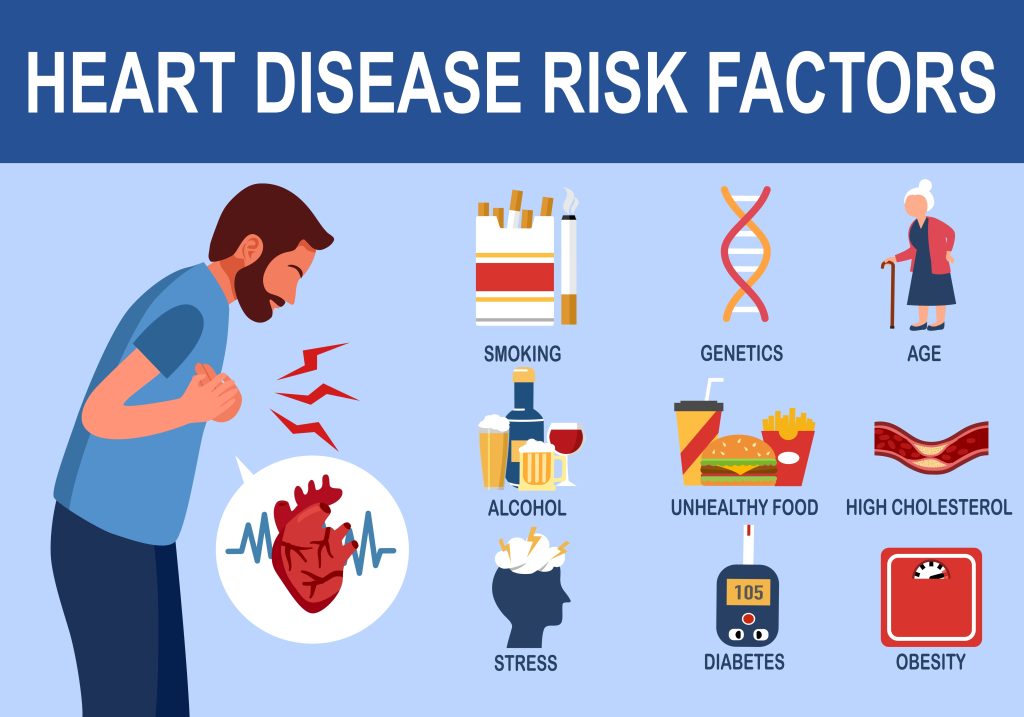
Generally speaking, a risk factor for a particular ailment merely means that there is a statistical correlation between the factor and the ailment. The risk factor could be strongly connected to a cause of the ailment. For example, impure drinking water is a risk factor for a host of infectious diseases. That’s because the organisms that cause those diseases breed in and are transmitted to humans through the impure water. Thus eliminating that risk factor by purifying drinking water has a significant positive effect on preventing infectious diseases. Similarly, in the United States, reducing smoking and air pollution has had a positive effect on the incidence of a number of aging-associated degenerative diseases. Those risk factors are not necessarily the root cause of the degenerative diseases (because even one who is not exposed to those risk factors can develop the same disease), but the risk factors accelerate the rate at which the diseases manifest themselves.
Attacking “Aging” as an Approach to Age-Associated Degenerative Disease
The term “Longevity Dividend” was coined by Professor S. Jay Olshansky and a group of scientists and academicians to describe “the economic and health benefits that would accrue to individuals and societies if we extend healthy life by slowing the biological processes of aging… [T]he idea is to slow the aging of our bodies such that 1 year of clock time is matched by less than 1 year of biological time. This approach would allow people to retain their youthful vigor for a longer time period and, if delayed-aging interventions work the way researchers hope they do, compress the infirmities of old age into a shorter time frame at the end of life.”¹
Extreme caloric reduction has been shown to have a life extending effect on mice. However, one cannot simply assume that an intervention that is successful on mice is going to work on humans.² There is also no reason to believe that something that extends the lifespan of a mouse is necessarily going to reverse cellular and tissue damage in young human adults. Caloric reduction slows the metabolism of mice, thus slowing the rate at which damage accumulates. The damage side of the equation is far more significant to a mouse than it is to a human. A mouse that has doubled its lifespan still lives only a few years. That’s because a mouse’s maintenance system is not nearly as sophisticated as a human’s. If humans were designed to live only a few years, then a radical slowing of metabolism might have an appreciable effect on longevity. But that’s not the case. Humans live much longer than mice (or apes for that matter) because humans have a much more well developed maintenance system.
The SENS Research Foundationi has a different approach to solving the problem. The SENS Research Foundation’s strategy is to prevent and reverse age-related ill health by applying the principles of regenerative medicine. According to its website, it is developing regenerative therapies that remove, repair, replace, or render harmless the cellular and molecular damage that accumulates in human tissues over time.³
- Olshansky SJ, Articulating the case for the longevity dividend, Cold Spring Harbor Perspectives in Medicine (2016).
- Where the disorder is caused by a pathogen invading the organism, it’s not unreasonable to assume that a pharmaceutical intervention that counteracts the pathogen in a lab rat is also likely to counteract the same pathogen in a human. However, when the disorder (FDS) is caused by an external factor interfering with the optimal functioning of the human maintenance system, assuming that an intervention that slows the rate at which intrinsic damage is inflicted upon lab rats will necessarily benefit humans is nonsensical.
- The SENS Research Foundation’s website is located at www.sens.org.
The next essay in this Section is “Pharmaceutical Interventions for Age-Associated Disorders.”